Global Health Matters
Obesity & Metabolism
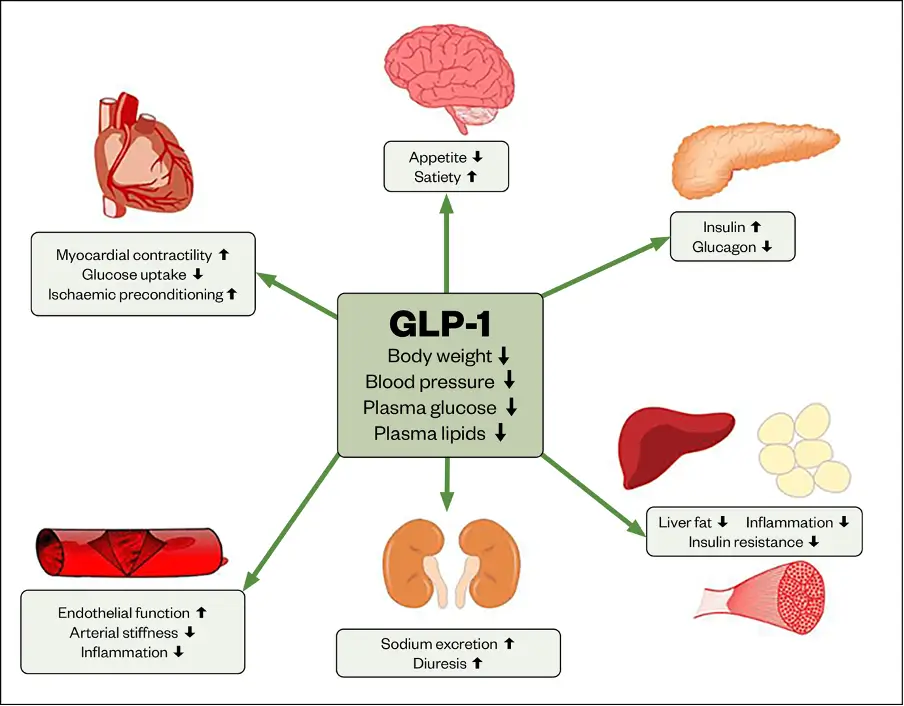
GLP-1, or glucagon-like peptide-1, is a hormone made by your intestines that plays a key role in controlling blood sugar and appetite.
When you eat, GLP-1 helps your body release insulin, which lowers your blood sugar.
It also helps you feel full, reduces how much sugar your liver produces, and slows down how fast food leaves your stomach.
These combined actions make GLP-1 very useful for managing diabetes and helping with weight loss.
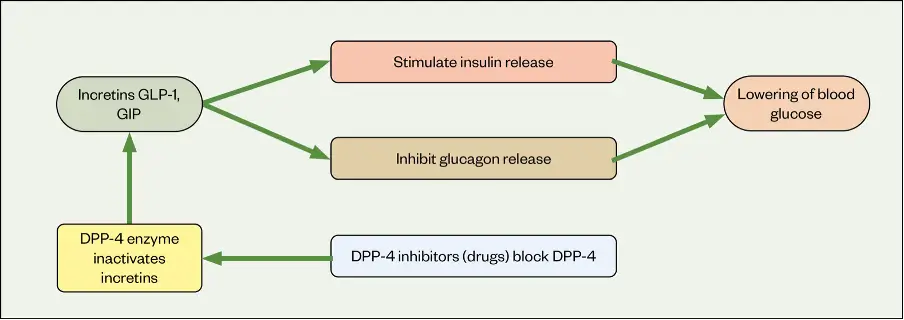
In healthy people, GLP-1 and another hormone called GIP help the body respond properly to food by increasing insulin.
But in people with type 2 diabetes, this process doesn’t work as well.
GLP-1 medicines (called receptor agonists) are used to restore this natural effect.
These medications not only improve insulin response, but also help control blood sugar after meals, reduce hunger, and may even help protect the cells in the pancreas that make insulin.
In addition, GLP-1 medicines may slow down stomach emptying, reduce the production of a hormone called glucagon (which raises blood sugar), and protect the heart and kidneys in some patients with diabetes.
Mechanisms by which GLP-1 analogues exert beneficial effects
Helps the Body Make More Insulin After Eating
When we eat, hormones like GLP-1 and GIP help the pancreas release more insulin to lower blood sugar. This natural response is called the incretin effect.
Breaks Down Quickly in the Body
These helpful hormones do not last long because they are broken down quickly by an enzyme called DPP-4.
Weaker Effect in Type 2 Diabetes
In people with type 2 diabetes, this natural process doesn’t work as well, which means the body struggles to make enough insulin after meals.
Medicines Can Restore This Effect
Medicines that act like GLP-1 can bring back this effect, helping people with diabetes make more insulin and control their blood sugar better.
Other Health Benefits of GLP-1 Medicines
– They slow down how fast food leaves the stomach, which helps keep blood sugar from spiking after meals.
– They lower the amount of another hormone (glucagon) that raises blood sugar when it’s already high.
– They may protect the pancreas by keeping its insulin-producing cells healthier for longer.
The effects of glucagon-like peptide in human physiology
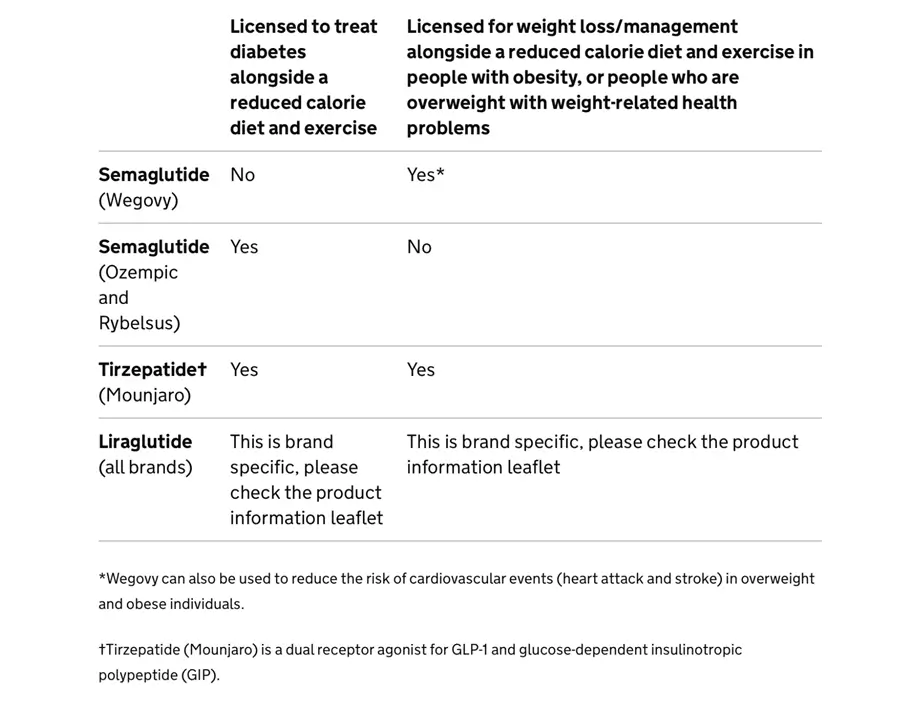
People with a BMI over 30 (classified as obesity) can benefit from GLP-1 medicines.
People with a BMI between 27 and 30 (overweight) may also qualify if they have at least one other weight-related health problem, such as diabetes, high blood pressure, or heart disease.
For people from South Asian, Chinese, Black African, or Caribbean backgrounds, the BMI limits are set lower by about 2.5 points, because they tend to develop health problems at lower weights compared to others.
Common Side Effects
Loss of Appetite: Often intentional for weight loss but may lead to reduced caloric intake.
Nausea: Frequently occurs, especially during the initial weeks of treatment.
Vomiting: Common, particularly when starting therapy or increasing doses.
Diarrhoea: A frequent gastrointestinal side effect that typically resolves over time.
Rare but Serious Risks
Pancreatitis: Acute pancreatic inflammation, though uncommon, requires immediate medical attention.
Acute Kidney Injury: Can occur, particularly in patients with pre-existing renal issues or dehydration.
Worsening Diabetic Retinopathy: Rapid glucose lowering may exacerbate pre-existing eye conditions in some patients.
Medullary Thyroid Cancer: A rare risk observed in animal studies, leading to caution in patients with a personal or family history of thyroid tumors.
Additional Considerations
Gastrointestinal Intolerance: Side effects like nausea and vomiting may lead to discontinuation if not managed with dose titration or supportive care.
Contraindications: GLP-1 agonists are not recommended in patients with severe gastrointestinal issues (e.g., gastroparesis), severe renal impairment, pregnancy, history of pancreatitis, or thyroid tumors, as these conditions increase the risk of adverse events.
Benefits
Enhance glucose-dependent insulin secretion: improve postprandial insulin response.
Suppress inappropriate glucagon secretion: reduce hepatic glucose output when blood sugar is high.
Delay gastric emptying: slow down absorption of glucose, blunting postprandial glucose spikes.
Promote weight loss: reduce appetite and food intake by acting on the hypothalamus.
Preserve β-cell function: reduce β-cell apoptosis and may promote proliferation.
Cardiovascular benefits: some agents have demonstrated reduction in major adverse cardiovascular events (MACE) in patients with T2DM and high cardiovascular risk.
Potential renal benefits: some evidence suggests reduction in albuminuria and slowing of kidney disease progression.
Personal or family history of Medullary Thyroid Carcinoma (MTC)
GLP-1 RAs carry a boxed warning (in the US) for risk of thyroid C-cell tumors.
Although the data come from rodent studies and human risk is not proven, they are contraindicated in patients with a personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Multiple Endocrine Neoplasia type 2 (MEN2)
Because MEN2 is associated with MTC, GLP-1 RAs are contraindicated.
Severe Gastrointestinal Disease
GLP-1 RAs slow gastric emptying and can exacerbate gastroparesis.
In patients with gastroparesis, severe GERD, or intestinal obstruction, these medications are usually avoided or used with caution.
History of Pancreatitis
There have been reports of acute pancreatitis in patients using GLP-1 RAs.
Although causality is debated, many guidelines advise against use in patients with a history of pancreatitis.
End-Stage Renal Disease (ESRD)
Some GLP-1 RAs (especially exenatide) are contraindicated in severe renal impairment (e.g., eGFR <30 mL/min/1.73m²).
Others (like liraglutide) may be safer but still require caution.
Pregnancy & Lactation
Data are insufficient to establish safety.
Generally not recommended in pregnancy insulin is preferred if glycaemic control is needed.
Hypersensitivity to the Drug
Any prior severe hypersensitivity reaction (e.g., anaphylaxis, angioedema) to the drug or any of its components is a contraindication.
Patients with severe depression or suicidal ideation (some post-marketing reports of mood changes exist).
Elderly patients, due to higher risk of GI side effects and dehydration.
Combination with insulin or sulfonylureas, due to risk of hypoglycaemia (though the GLP-1 RA itself rarely causes hypoglycaemia).